What is metabolic health? A biochemist’s definition
It depends on who you ask, but there are some generally agreed upon parameters for measuring metabolic health. It can be measured in our blood or bodies. These medical, physiological and laboratory test markers can indicate if intricate body processes are working normally. However, we don’t have to understand the detailed metabolic processes to benefit from measuring them.
How does the biochemist who wrote Nutrition in Crisis define metabolic health?
We asked Professor Richard Feinman, PhD, who kindly provided us a comprehensive, scientific explanation:
- Metabolic health is the absence of metabolic disease. Evolution only selects for those who can keep their metabolism going until the next generation.
- In turn metabolic disease is defined by diseases whose symptoms can be corrected by metabolic treatment. Usually, therapies are based on controlling the input (diet) or the machinery (enzymes and hormones).
- Increasingly, we see different diseases that respond to such approaches. But in the end, diabetes remains the exemplar of a metabolic disease. For example, the argument that cancer can be viewed as a metabolic disease rests in part on the similarities to diabetes.(1), (2)
- Diabetes remains a disease of disruption of the glucose-insulin axis but the effects are seen in global metabolic changes.(3)
- Several assays of the condition have been developed including:
- Oral Glucose Tolerance Test (OGTT) (as first proposed by Dr Joseph Kraft)
- Oral Lipid Tolerance Test (OLTT)
- Lipopolysaccharide (LPS) challenges.
Wow. Let’s unpack that a little, or see our plain language definition of metabolic health.
Does metabolic syndrome help us define metabolic health?
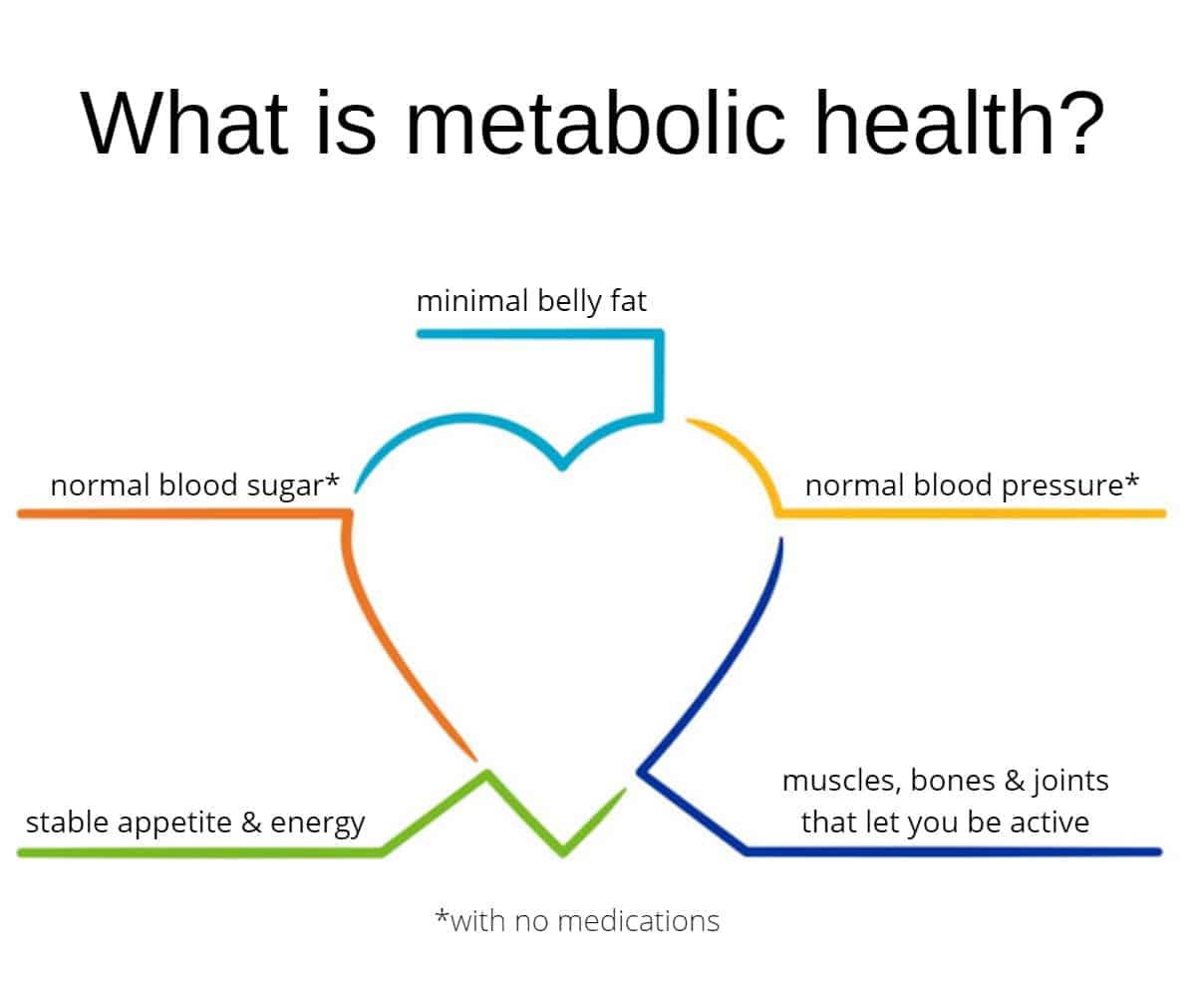
Heard of metabolic syndrome? It is defined here by the American Heart Association as occurring when a person has three or more of the following measurements:
- Abdominal obesity (Waist circumference greater than 40 inches in men, and greater than 35 inches in women)
- From your blood-work
- Triglyceride level of 150 milligrams per deciliter of blood (mg/dL) or greater
- HDL cholesterol of less than 40 mg/dL in men or less than 50 mg/dL in women
- Systolic blood pressure (top number) of 130 millimeters of mercury (mm Hg) or greater, or diastolic blood pressure (bottom number) of 85 mm Hg or greater without medication
- Fasting glucose of 100 mg/dL or greater(4)
How prevalent is metabolic health?
Metabolic Syndrome is a description of disordered metabolism. Now let’s compare Metabolic Syndrome with metabolic health. According to a recent study, metabolic health was defined relative to the 5 criteria above for metabolic syndrome. The study applied these current guidelines to a very large U.S. data set, the National Health and Nutrition Examination Survey (NHANES). For blood pressure (BP) they applied a slightly lower cut off, systolic BP <120 and diastolic BP <80 mmHg.(5)
Only 1 in 8 Americans is metabolically fit?
Yes. According to this NHANES study, only 12% of Americans are considered metabolically healthy.
That is, only 3 out of every 25 people have the following:
- an ideal waist measurement,
- are not prediabetic in their blood sugar
- a normal, not hypertensive blood pressure,
- normal blood fats (triglycerides & HDL), and
- do not take medications for any of these issues. Wow. The study concluded:
The prevalence of metabolic health in American adults is very low, even in normal weight individuals. The large number of people not achieving optimal cardiometabolic levels of risk factors has serious implications for public health.”
(Araújo 2019)(6)
What is metabolism?
Metabolism is basically every chemical process in your body necessary for the maintenance of life! It is the biological theory of everything!
- Energy production? Metabolism.
- Building new tissues? Metabolism.
- Breaking down old tissue to repair it? Metabolism.
- Elimination of waste? Metabolism.
- Growth? Metabolism.
- Cellular reproduction? Metabolism.
- Warding off disease? Metabolism.
You get the idea? It is everything your body does. So Metabolic Syndrome is very serious. It can impact all the varied functions of your body. Conversely, metabolic health is also important as it can optimize all these same functions making you run like a well-oiled machine!
Why do we have such poor metabolic health?
- Read our post Americans Can’t Afford to Wait Any Longer. It’s Time to Overhaul the U.S. Dietary Guidelines.
How can I improve my metabolic health?
Start with what our grandparents knew was healthy.
- Eat a diet of whole foods. Reduce sugar and processed foods. Minimize stress eating and snacking.[Feinman]
- Get adequate, restful sleep.
- Maintain or increase your level of exercise. Consult your physician!
- Reduce stress. That includes stressing about stress.
- Don’t eat from dinner to breakfast or lunch. Also known as Time Restricted Eating or TRE.
- Get plenty of sunshine, fresh air and nature.
- Maintain your positive social networks (at a distance).
- Cultivate contentment. This might be through spirituality, meditation, a gratitude practice a hobby like gardening, or turning off the news.
- Practice a Growth Mindset. Learn something new (Best keto resources) or read a book.
- Avoid smoking, excess alcohol and drugs.
- Find a clinician you can partner with. (Keto doctors near me)
- If you’re overwhelmed, pick one area and work on that. You might be surprised at how fixing one thing can synergize everything else!
For more ideas see these lifetime learning ideas.
How can I understand my bio-individuality?
- Consider wearing a continuous glucose monitor. What happens after you eat? Do you have high blood glucose when you wake up (“dawn phenomenon”)? Why do some meals seem to not affect my blood sugar very much? What’s the variability in your blood glucose levels during the day?(7)
- A blood pressure cuff is an inexpensive addition to your tool-kit. As we’ve mentioned, high BP is part of metabolic syndrome.
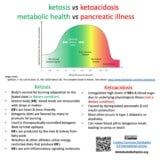
- What about ketones? A ketone meter often has a dual capability to use glucose strips as well. What happens to your ketone bodies after exercising? If you try time restricted eating (skip a meal), then how does your ketone measurement change?
- A simple tape measure can provide an indication that your lifestyle modifications are progressing as you desire. Weighing yourself can be more of an indicator of water retention or loss than of actual body mass reduction.
- More detailed InBody™ metrics can be obtained from machines usually found at athletic clubs and gyms. They provide more accurate information than a weight scale and don’t require blood samples.
David S. Ludwig, MD
Dr. Ludwig, MD, PhD, is a practicing endocrinologist, researcher, and professor at Harvard Medical School and Harvard School of Public Health. He also directs the New Balance Foundation Obesity Prevention Center at Boston Children’s Hospital. His research focuses on how food affects hormones, metabolism, body weight, and well-being. He co-authored
- “Americans Are Already Too Diseased to Go Back to Work Right Now: The huge burden of obesity and other chronic conditions among people in the U.S. puts most of us at direct risk.” in the New York Times.
Kristin Baier, MD
Dr Baier, MD, is board certified in both Family and Obesity Medicine. practices as part of Low Carb MD San Diego‘s Direct Primary Care practice. She shared these insightful observations:
The consequences of metabolic syndrome range from Type 2 diabetes, increased risk of cardiovascular disease and more severe complications from infections. The good news is, favorable metabolic changes are appreciated in only 3 weeks, sometimes less. In these uncertain times, empowerment can be found in making decisions that benefit your health to reduce risk of morbidity and mortality. Eliminating foods that induce hyperglycemia and inflammation are a great start to improving your metabolic health
Kristin Baier, MD 14 May 2020
Is there any metabolic health research that I might participate in?
Below are two such research projects. If you find others, then please let us know.
“Meterbolic” – The importance of measuring insulin resistance (IR)
Gabor Erdos & Eric Smith are using metabolic measurement analytics to better understand insulin resistance over an 18 month long project. “Metabolic health, or as it is often called, metabolic flexibility, is commonly characterized by measuring insulin resistance (IR). The basic definition of IR is the alteration of observed nutrient clearance speed from the blood. I say observed, because any snapshot level is the result of processes that remove, but also of those that add nutrients to the blood.
Due to the highly dynamic nature of nutrient levels, any single measurement provides limited information. Often, determining the concentrations of two or more molecules that are in a close relationship, but delayed in time, can provide additional input to confer the underlying dynamics. Moreover, deterioration of fasting and postprandial (= after meal) levels of nutrients and hormones can be largely disconnected.”
Gabor Erdosi & Eric Smith – Meterbolic
Cholesterol Code – Reverse Engineering the Mystery
Another endeavor exploring metabolic health is the Citizen Science Foundation and its central endeavor, the LMHR Measurement Project. It has evolved out of Dave Feldman and Siobhan Huggin’s work at Cholesterol Code. Currently, their Lean Mass Hyper-Responder [LMHR] project focuses on lipid profiles. Most LMHRs are fit in every aspect, but one. Because they are on very-low carbohydrate or ketogenic diets their blood-work often presents a paradox:
very low triglycerides with very high cholesterol.
Are there people out there that want high cholesterol?
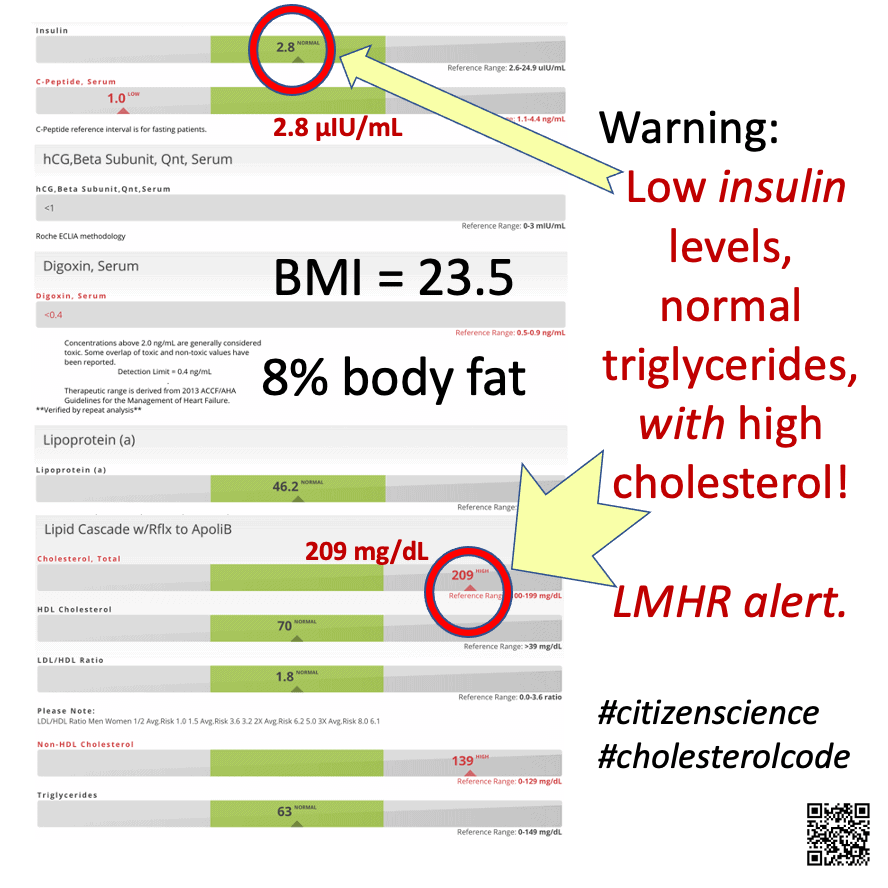
The LMHR Measurement Project uses anonymized data for their analysis. Here is a recent example excerpt provided by Mani Malagón, who is happy he fits the LMHR profile.(10),(11) The blood work results were obtained through Cholesterol Code and the BMI and percent body fat results came from an InBody™ machine. For our discussion on body composition and the importance of skeletal muscle (lean body mass) on basal metabolic refer to this summary graph.
What’s a lean mass hyper-responder (LMHR)?
The Lean Mass Hyper-responder (LMHR) phenotype is characterized by LDL cholesterol of 200 mg/dL or higher, HDL-C of 80 mg/dL or higher, and Triglycerides of 70 mg/dL or lower. They are likewise interested in “borderline” LMHRs that are near these same cut points.
What other areas are Cholesterol Code and Citizen Science Foundation looking at?
Dave and Siobhan are working to
[P]rovide wide spectrum blood panels and cardiovascular testing such as CT Angiogram, Carotid Intima Media Thickness (CIMT), and Coronary Artery Calcium (CAC) score to this phenotype of interest where we likewise confirm no genetic Familial Hypercholesterolemia.
Cholesterol Code
By the way, Cholesterol Code is developing a data collection tool (CholesterolCode Report Tool v0.9.5.15) where you might want to provide data for their continuing studies. Do you think we’ll be shifting from worrying about cholesterol to perhaps looking at a triglyceride and glucose index (TyG)? Such an index could give insights about insulin resistance and non-alcoholic fatty liver disease (NAFLD).(12),(13)
You might want to try the TyG calculator provided at Burn Fat Not Sugar.
Are leading thinkers redefining health?
Yes. Examples include positive health and phenotypic flexibility. P4 health advocates for an integrative vision of physical, mental and spiritual health while including complex factors that influence metabolic health.
Positive health
Positive health shifts the narrative from the current emphasis on intervention and remediation. It emphasizes maintaining metabolic health and preventing chronic diseases.(14),(15),(16),(17)
Phenotypic flexibility
The European Commission has funded the “Nutritech” project. It will explore the “Application of new technologies and methods in nutrition research – the example of phenotypic flexibility.” It is based on
‘phenotypic flexibility’, based on metabolic flexibility (the capacity for the organism to adapt fuel oxidation to fuel availability)”(18) ,(19)
“P4 Health or O4 Medicine? Hippocrates provides the answer
P4 Health – ( Predictive, Preventative, Personalized, Participatory) “provides a framework to detect and prevent disease.” They define O4 medicine as Overtesting, Overdiagnosis, Overtreatment, Overpayment.(20)
Do I have to improve my lifestyle or can I just take a pill instead?
Metabolic syndrome, obesity and diabetes are common and often occur together. Unfortunately, metabolic syndrome and obesity alone don’t do a great job of predicting or classifying diabetes. Other risk factors are involved.(21) Would many of us benefit from embracing lifestyle medicine?
My thanks to Mani Malagon and Christie Barnett who both provided substantial research. Professor Richard Feinman for kindly providing his input. Mani Malagon was also my Fact Checker.
Sources:
- 1. Fine, et al. (2012) Targeting insulin inhibition as a metabolic therapy in advanced cancer: a pilot safety and feasibility dietary trial in 10 patients. Nutrition. 28, 1028-1035.[↩]
- 2. Fine, EJ and Feinman, RD (2014) Insulin, Carbohydrate Restriction, Metabolic Syndrome and Cancer. Expert Review of Endocrinology & Metabolism. 9, 1-10[↩]
- 3. Feinman, R.D. (2019). Nutrition in Crisis, Chelsea Green Publishing: White River Junction, VT, 167-72[↩]
- 4. Similar guidelines are used by the AACE. Screening and Monitoring of Prediabetes | American Association of Clinical Endocrinologists. (n.d.). Retrieved May 8, 2020, from https://www.aace.com/disease-state-resources/diabetes/depth-information/screening-and-monitoring-prediabetes[↩]
- 5. Araújo, J., Cai, J., & Stevens, J. (2019). Prevalence of Optimal Metabolic Health in American Adults: National Health and Nutrition Examination Survey 2009-2016. Metabolic Syndrome and Related Disorders, 17(1), 46–52. https://doi.org/10.1089/met.2018.0105[↩]
- 6. Ibid.[↩]
- 7. Feinman, R. D., Pogozelski, W. K., Astrup, A., Bernstein, R. K., Fine, E. J., Westman, E. C., Accurso, A., Frassetto, L., Gower, B. A., McFarlane, S. I., Nielsen, J. V., Krarup, T., Saslow, L., Roth, K. S., Vernon, M. C., Volek, J. S., Wilshire, G. B., Dahlqvist, A., Sundberg, R., Childers, A., Morrison, K., Manninen, A. H., Dashti, H. M., Wood, R. J., Wortman, J., & Worm, N. (2015). Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition, 31(1), 1-13. https://doi.org/10.1016/j.nut.2014.06.011[↩]
- 10. Ramsden, C. E., Zamora, D., Majchrzak-Hong, S., Faurot, K. R., Broste, S. K., Frantz, R. P., Davis, J. M., Ringel, A., Suchindran, C. M., & Hibbeln, J. R. (2016). Re-evaluation of the traditional diet-heart hypothesis: analysis of recovered data from Minnesota Coronary Experiment (1968-73). BMJ, 353, i1246. http://doi.org/gcpfmt[↩]
- 11. Ravnskov, U., Diamond, D. M., Hama, R., Hamazaki, T., Hammarskjöld, B., Hynes, N., Kendrick, M., Langsjoen, P. H., Malhotra, A., Mascitelli, L., McCully, K. S., Ogushi, Y., Okuyama, H., Rosch, P. J., Schersten, T., Sultan, S., & Sundberg, R. (2016). Lack of an association or an inverse association between low-density-lipoprotein cholesterol and mortality in the elderly: a systematic review. BMJ Open, 6(6), e010401. http://doi.org/f3rsq9[↩]
- 12. Simental-Mendía,L. E., Rodríguez-Morán, M., & Guerrero-Romero, F. (2008). The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord, 6(4), 299-304. http://doi.org/ck8hj7[↩]
- 13. Zhang, S., Du, T., Zhang, J., Lu, H., Lin, X., Xie, J., Yang, Y., & Yu, X. (2017). The triglyceride and glucose index (TyG) is an effective biomarker to identify nonalcoholic fatty liver disease. Lipids in health and disease, 16(1), 15. http://doi.org/dvp8[↩]
- 14. Huber, M., van Vliet, M., Giezenberg, M., Winkens, B., Heerkens, Y., Dagnelie, P. C., & Knottnerus, J. A. (2016). Towards a ‘patient-centred’ operationalisation of the new dynamic concept of health: a mixed methods study. BMJ Open, 6(1), e010091. https://doi.org/10.1136/bmjopen-2015-010091[↩]
- 15. Luxford, K. (2016) ‘First, do no harm’: shifting the paradigm towards a culture of health, Patient Experience Journal: 3:2;2. http://doi.org/dvnc[↩]
- 16. Minihane, A. M., et al. (2015). Low-grade inflammation, diet composition and health: current research evidence and its translation. British Journal of Nutrition, 114(7), 999-1012. http://doi.org/f7s8kw [↩]
- 17. Vauzour, D., et al. (2017). Nutrition for the ageing brain: Towards evidence for an optimal diet. Ageing Res Rev, 35, 222-240. http://doi.org/br28[↩]
- 18. Application of new technologies and methods in nutrition research – the example of phenotypic flexibility | NUTRITECH Project | FP7 | CORDIS | European Commission. (n.d.). Retrieved May 12, 2020, from https://cordis.europa.eu/project/id/289511[↩]
- 19. Stroeve, J. H. M., van Wietmarschen, H., Kremer, B. H. A., van Ommen, B., & Wopereis, S. (2015). Phenotypic flexibility as a measure of health: The optimal nutritional stress response test. Genes & Nutrition, 10(3). https://doi.org/10.1007/s12263-015-0459-1[↩]
- 20. Fiala, C., Taher, J., & Diamandis, E. P. (2019). P4 Medicine or O4 Medicine? Hippocrates Provides the Answer. The Journal of Applied Laboratory Medicine, 4(1), 108–119. https://doi.org/10.1373/jalm.2018.028613[↩]
- 21. Lotta, L. A., Abbasi, A., Sharp, S. J., Sahlqvist, A.-S., Waterworth, D., Brosnan, J. M., Scott, R. A., Langenberg, C., & Wareham, N. J. (2015). Definitions of Metabolic Health and Risk of Future Type 2 Diabetes in BMI Categories: A Systematic Review and Network Meta-analysis. Diabetes Care, 38(11), 2177-2187. https://doi.org/10.2337/dc15-1218[↩]







I enjoyed this article. Article brought to my mind some thoughts that I wish to share. In particular a bio-individuality addressed . If a healthy metabolism is a result of the healthy living, how we may define metabolism of the person whom is coping with own pathology while desperately tries to reach out for the “healthy” values of lucky one?.. His or her values would be well different from healthy subject and might never reach the defined “normal” … An obsessive comparing of the own data with “normal” one, would create further stress and will deep the disappointment, or possibly create sensation of failure from the beginning.. This why 4Ps are so crucial in elaborating personalized plan of actions. Lately, we have been achieving in our goal of the population longevity, but our current situation clearly shows we are failing in quality who made it?…Recovery from the metabolic syndrome may take longer that it might be expected by the subject. Realistic plan of actions shell focus on living this metabolic health journey, instead of fighting for a ” healthy” value in some kind metabolic boot camp… Sometimes, we have to accept the reality we are not able to change and stop fighting our “demons”.. Accepting own limitation is not a weakness but may give a moment of revelation..
Mantra,
Great points & I’m glad you enjoyed it. Yes, bio-individuality does argue for improving against one’s own markers. While biome research is in it’s infancy, so far it is emphasizing the complexity of all factors affecting each person’s metabolism. Did you have a life-saving, high dose of antibiotics as a child? Have you been athletic most of your life? Do you internalize stress or have you experienced trauma.
Recovering from metabolic syndrome takes longer for some. I love your image of “living this metaboiic journey” in contrast to arriving at a metabolic health destination. Perhaps that’s why the clinicians and researchers want to define it in terms of what metabolic health is not vs. a state that one achieves.
Great food for though in your comment. Thank you! — Cecile
Mantra,
You make several very valid points. Our modern lifestyle has created conditions that seem to lead inevitably to chronic illness; and consider aging as inevitably associated with medical conditions.
That being said, there is a fresh wind of new opinions and ideas about how to prevent and often reverse the illness that we have come to take for granted. We are on a journey of exploration of, sometimes ancient, but now scientifically validated concepts to help us improve our metabolic flexibility. It is a shift from our sick-care orientation to one of health-care. We are attempting to curate the best information that has been validated by scientific methods and make it available.
Thank you for your thoughtful insights.